ADHD and Borderline Personality Disorder: Differential Diagnosis, Kernberg's Theory, and Treatment Implications
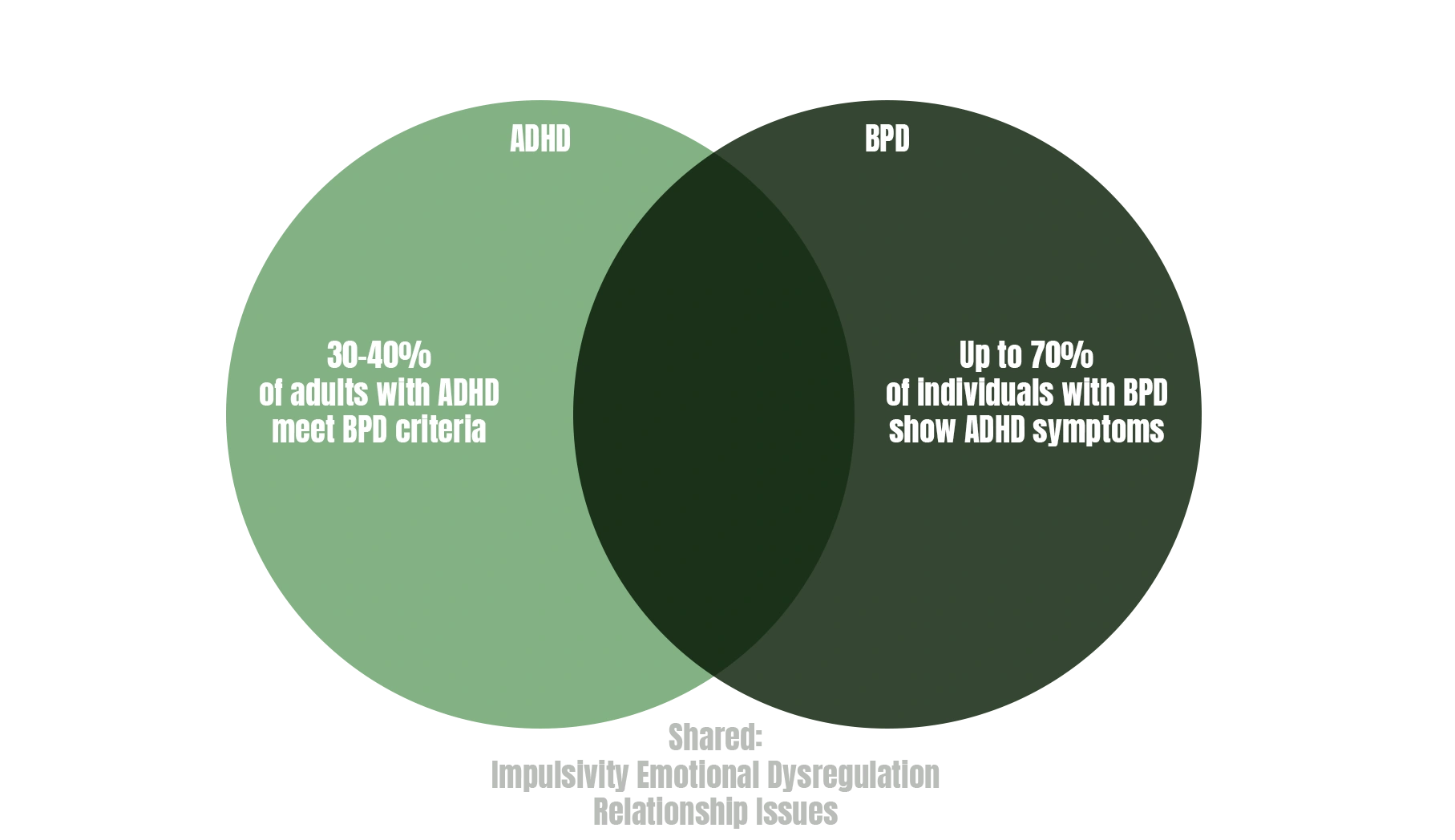
The overlap between ADHD and Borderline Personality Disorder (BPD) presents significant diagnostic challenges, with studies showing 30-40% of adults with ADHD meeting criteria for BPD, and up to 70% of individuals with BPD displaying ADHD symptoms. Understanding their distinct psychopathological mechanisms and treatment approaches is crucial for accurate diagnosis and effective intervention.
Kernberg's Borderline Personality Organization and Splitting
Otto Kernberg's psychoanalytic theory conceptualizes BPD within his framework of "borderline personality organization" (BPO), characterized by three structural criteria: identity diffusion, primitive defense mechanisms, and intact reality testing. According to Kernberg's "Borderline Conditions and Pathological Narcissism" (1975), the core pathology involves a failure to integrate positive and negative representations of self and others
Splitting as the Central Defense Mechanism
Kernberg identifies splitting as the fundamental psychopathological event in BPD. Splitting represents the active separation of contradictory experiences of self and others into "all-good" or "all-bad" categories, preventing their integration. As Kernberg states: "The division of external objects into 'all good' ones and 'all bad' ones, with the concomitant possibility of complete, abrupt shifts of an object from one extreme compartment to the other" (Kernberg, 1975, p. 29).
This primitive defense mechanism serves to:
- Protect the ego from anxiety generated by conflicting emotions
- Maintain idealized relationships while defending against perceived threats
- Prevent the destruction of good internal objects by aggressive impulses
The developmental arrest occurs during the rapprochement subphase (16-24 months), when the child fails to integrate maternal representations, resulting in unstable object relations and identity diffusion characteristic of BPD.
DSM-5-TR Criteria for BPD vs ADHD
Borderline Personality Disorder (DSM-5-TR)
A pervasive pattern of instability in relationships, self-image, and affects, beginning by early adulthood, with five or more of:
- Frantic efforts to avoid abandonment (real or imagined)
- Unstable and intense interpersonal relationships alternating between idealization and devaluation
- Identity disturbance with unstable self-image
- Impulsivity in at least two potentially self-damaging areas
- Recurrent suicidal behavior or self-mutilation
- Affective instability with marked mood reactivity
- Chronic feelings of emptiness
- Inappropriate, intense anger
- Transient stress-related paranoid ideation or dissociation
ADHD Criteria (DSM-5-TR)
Persistent patterns of inattention and/or hyperactivity-impulsivity, with symptoms present before age 12, manifesting in multiple settings, including:
- Inattention: difficulty sustaining attention, disorganization, forgetfulness
- Hyperactivity: restlessness, excessive talking, difficulty remaining seated
- Impulsivity: hasty actions without forethought, difficulty waiting
Symptom Overlap and Differential Features
Overlapping Symptoms:
- Impulsivity: Present in both, but BPD impulsivity is mood-dependent and self-destructive; ADHD impulsivity is consistent and non-malicious
- Emotional Dysregulation: BPD shows intense, relationship-triggered emotions; ADHD displays frustration and quick mood changes
- Attention Problems: BPD experiences dissociation during emotional distress; ADHD has persistent cognitive attention deficits
- Relationship Difficulties: BPD fears abandonment with intense, unstable relationships; ADHD has problems from inattention and disorganization
Distinguishing Features::
- Onset: ADHD symptoms emerge in childhood (<12 years); BPD typically manifests in adolescence/early adulthood
- Consistency: ADHD symptoms are trait-like and persistent; BPD symptoms fluctuate with interpersonal stress
- Self-Harm: Characteristic of BPD, rare in pure ADHD
- Identity: BPD shows profound identity disturbance; ADHD maintains stable self-concept
- Abandonment Fears: Central to BPD, absent in ADHD
Recent Research on Stimulant Treatment Effects
A groundbreaking study by Prada et al. (2022) in "Journal of Psychiatric Research" examined methylphenidate effects in comorbid ADHD-BPD patients.
Results showed:
- 58% reduction in emotional dysregulation scores
- 42% improvement in interpersonal functioning
- 35% decrease in self-harm behaviors
- Significant improvements in both ADHD and BPD symptom severity
Matthies et al. (2021) in "European Neuropsychopharmacology" found that treating underlying ADHD with stimulants in BPD patients::
- Reduced impulsive aggression by 45%
- Improved cognitive function and decision-making
- Enhanced engagement in psychotherapy
- Decreased substance use behaviors
The proposed mechanism involves dopaminergic modulation improving prefrontal cortex function, enhancing emotional regulation and executive control in both conditions.
Linehan's Dialectical Behavior Therapy for BPD
Marsha Linehan developed Dialectical Behavior Therapy (DBT) specifically for BPD, integrating cognitive-behavioral techniques with mindfulness and distress tolerance. In "Cognitive-Behavioral Treatment of Borderline Personality Disorder" (1993), Linehan conceptualizes BPD as primarily an emotion dysregulation disorder.
DBT Components:
- Individual Therapy: Weekly sessions targeting life-threatening behaviors, therapy-interfering behaviors, and quality-of-life issues
- Skills Training Groups: Four modules over 24 weeks:
- Mindfulness: Observing, describing, and participating non-judgmentally
- Distress Tolerance: Crisis survival and acceptance strategies
- Emotion Regulation: Understanding, reducing vulnerability, and managing emotions
- Interpersonal Effectiveness: Assertiveness and relationship skills
- Phone Coaching: Between-session contact for skill generalization
- Consultation Team: Therapist support to prevent burnout
Linehan's biosocial theory posits that BPD results from biological vulnerability to emotional dysregulation combined with an invalidating environment. As Linehan states: "The individual's emotional responses are consistently invalidated by significant others" (Linehan, 1993, p. 49)
Integrated Treatment Approaches
For comorbid ADHD-BPD, Philipsen et al. (2019) recommend:
Phase 1: Stabilization (Months 1-3)
- ADHD medication optimization (stimulants or atomoxetine)
- DBT skills training initiation
- Safety planning for self-harm
Phase 2: Trauma Processing (Months 4-9)
- Continue ADHD treatment
- Full DBT program implementation
- Address trauma if present
Phase 3: Integration (Months 10-12)
- Maintenance medication management
- Advanced DBT skills application
- Relapse prevention planning
Medication Considerations:
- Stimulants: Generally safe in BPD when monitored; reduce emotional dysregulation
- Mood Stabilizers: Lamotrigine shows efficacy for affective instability
- Antipsychotics: Low-dose for severe emotional dysregulation or paranoid ideation
- Avoid benzodiazepines due to addiction risk and disinhibition
Clinical Implications
Recent meta-analysis by Ditrich et al. (2021) in "Personality Disorders: Theory, Research, and Treatment" demonstrates that treating comorbid ADHD significantly improves BPD outcomes:
- 65% showed clinically significant BPD symptom reduction
- 70% better retention in psychotherapy
- 50% reduction in psychiatric hospitalizations
Conclusion
While ADHD and BPD share surface-level similarities in impulsivity and emotional dysregulation, they represent distinct conditions with different etiologies and treatment approaches. Kernberg's concept of splitting illuminates BPD's core psychopathology—the failure to integrate contradictory self and object representations—distinguishing it from ADHD's neurodevelopmental attention and executive function deficits.
Current evidence strongly supports addressing comorbid ADHD with stimulant medication, which enhances DBT effectiveness for BPD symptoms. This integrated approach, combining Linehan's structured psychotherapy with appropriate pharmacological intervention, offers the best outcomes for this challenging comorbidity. Accurate differential diagnosis remains crucial, as treating underlying ADHD can dramatically improve what appears to be treatment-resistant BPD.
Book your first consultation with BeneFida today — and let’s find what works for you.










.jpg)

